Bladder anatomy
- Arterial supply: Superior and inferior vesical arteries (from internal iliac artery)
- Venous return: Vesical venous plexus (will see when bladder is lifted) -> internal iliac veins
- Nerve (sympathetic): sup/inf hypogastric plexus
- Nerve (parasympathetic): inf hypogastric plexus, pelvic splanchnic n.
- Lymphatic drainage
- Level I: interal iliac, obturator, external iliac
- Level II: common iliac, presacral
- 7% of the time bladder cancer can skip to level 2 without level 1 involvement
- Level III: para-aortic, interaortocaval, paracaval
- Generally have level I/II involvement as well
Radical cystectomy: Gold standard for muscle-invasive, non-metastatic bladder UC.
- Removal of bladder and pelvic lymph nodes, with prostate+seminal vesicles in men, or +/- anterior vagina+uterus/fallopians/ovaries in women
- Surgical video - robotic anterior exenteration/cystectomy
- Skinner cystectomy
- Surgical atlas - neobladder (PDF) (W shape Hautman; Skinner does U shape Studer)
- Indiana pouch - surgical steps, BCAN patient comments, tips from Indiana
- Indications
- Muscle-invasive cancer (T2 and above)
- Recurrent non-muscle-invasive (failed resection/intravesical BCG, esp. if failed 2x)
- High-grade T1 lesions a/w CIS/LVI/variant histologies (if long life expectancy, or multiple/large tumors)
- Partial cystectomy can be performed if able to achieve negative margins (eg bladder dome or diverticulum), no prior hx of bladder tumors, no prostate involvement
- **hide**But prostate cancer found in 23-54% of RC specimens; 17-75% had UC involving prostate
- **hide**Gynecologic UC involvement in < 5%
- Not recommended if able to have RC
- **hide**Intraoperative frozen-section of ureteral margin - negative margin after positive margin still had higher risk of upper tract recurrence; should still attempt for negative margin
Pelvic lymph node dissection (PLND) should be performed with radical and partial cystectomy.
- Standard PLND - up to level I (external iliac, internal iliac, obturator)
- Extended PLND - up to level II (common iliac, presacral)
- Super-extended PLND - up to level III (para-aortic, interaortocaval, paracaval)
- Extended/super-extended PLND traditionally thought to improve survival by removing more micrometastatic disease, but recent (2023) SWOG 1011 randomized phase 3 trial showed no survival benefit to extended dissection; increased toxicity (54% vs 44% adverse events, 7% vs 2% death within 90 days).
- Goal - 25-node minimum (75% chance of identifying 1+ LN metastasis; retrospective data)
- 15% of T2 (presumed N0) disease undergoing cystectomy will have node-positive disease
| Superior |
Limited - common iliac |
| Inferior | inguinal/Cooper's ligament |
| Medial | bladder/internal iliac |
| Lateral | pelvic side wall, genitofemoral nerve |
| Anterior | external iliac vein |
| Posterior | obturator nerve (extended - down to pelvic floor) |

Female anatomy - uterine artery
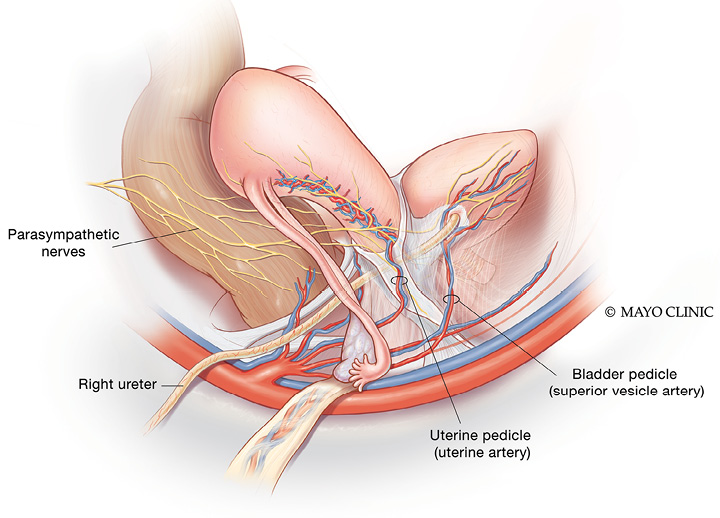
Internal iliac artery anatomy

Urinary diversion:
- No overall difference in QoL between methods, but limited data.
- Bowel prep (e.g. Nichols prep) not necessary if using small bowel.
- Ideal reservoir is
- Non-refluxing
- Refluxing ureteral anastomosis has lower stricture rate, but recommend anti-refluxing for continent diversion
- In intermediate term, anti-refluxing does not appear to be necessary for upper tract preservation or UTI prevention
- Low-pressure (detubularize the bowel)
- Continent
- Non-absorptive
- Non-refluxing
- Bricker (independent ureteral anastomosis) vs. Wallace (ureters spatulated and anastomosed together to ileum) : no difference in stricture rate.
- If using ileum, start ~15-20 cm proximal to ileocecal valve to preserve salt absorption.
| Cutaneous urinary diversion (ileal conduit) |
Non-continent Complications: parastomal hernia, stomal stenosis
|
|
| Catheterizable urinary diversion (Indiana pouch) |
Continent - Ileocecal valve provides the continence mechanism; use R colon as the reservoir (perform pre-op colonoscopy) 28 cm of R colon (detubularize into pouch), ~10 cm of ileum (taper into cath channel) |
Contraindications to continent diversion
Neobladder specific contradindications
|
| Neobladder |
Continent - void per urethra Complications:
|
|
| Ureterosigmoidostomy | Continent diversion to GI tract | Increased risk of colon cancer (urine is caustic) 2.5% at ~26 yrs. Begin colonoscopies at 10 years. Also increased risk with enterocystoplasty (augmentation), but not with other diversions. |
Complications of bowel in the urinary tract
- Depends on length of conduit, segment of intestine, duration of contact (continent vs non-continent)
| K | Cl | pH | Other | |
| Colon/ileum | ↓ | ↑ | acidosis | Compensates with bone buffer -> demineralization, growth impairment Treat with K citrate, or chloride blockers (chlorpromazine, nicotinic acid) Ileal resection: hyperoxaluria/stones, B12 deficiency (>5 years post-op. Start checking at 1 year; replete with sublingual B12) Start ~15-20 cm proximal to ileocecal valve to preserve salt absorption. Spina bifida patients need ileocecal valve for fecal continence |
| Kidneys eliminate acid by ammonium excretion, but colon/ileum reabsorbs ammonium (watch out if liver disease) |
||||
| Stomach |
↓ |
↓ |
alkalosis |
Treat with H2 blockers, PPI |
|
Gastric secretions (K, HCl) lost in urine |
||||
| Jejunum | ↑ | ↓ | acidosis (hyponatremic) |
Treat with NaCl hydration; correct hyperkalemic acidosis; long-term oral NaCl |
| Secretes NaCl, absorbs H, K (exacerbated with TPN) | ||||
Complications of conduit diversion (10-20%)
- Bowel - obstruction, fistula, abscess
- Renal failure
- Recurrent UTI (bowel is chronically colonized), pyelonephritis
- Parastomal hernia or stomal stenosis
- Anastomotic strictures
- Stones from UTI, mucus, acidosis/hypokalemia, dehydration from diarrhea
- Staple lines can be nidus for stones
- Mucus: colon > ileum > stomach; increased with dairy
- Diarrhea after bowel resection; treat with cholestyramine
- Renally excreted drugs can be reabsorbed
- Methotrexate - drain diversion during chemo; alkalinize the urine and hydrate
- Interesting technical article on PCNUs for conduit leaks
ERAS protocol (Early Recovery after Surgery) - hopsital stay 3-5 d instead of 8-10; early fluids/feeding. Entereg/almivopan - blocks narcotic effect on bowel
Stanford: ***update with new pathway
- Pre-op abx: cefoxitin
| Diet | Pain | Activity | Other | |
| POD 0 | clears IVF |
Tylenol, toradol, gaba, oxy Entereg |
OOB & amb, chair x 30 min | Neobladder: start q4h irrigation |
| POD 1 | PS1 SLIV |
Stop Entereg when having BMs | chair x 6-8 hrs, amb x 4-5 | Ileal conduit: stoma visits |
| POD 2 | reg | amb x 4-5 | ||
| POD 3-4 home |
Stents out by POD 4 (Skinner) Switch heparin to lovenox (30 d) POD 3-4
If neobladder, get urine culture before going home in case of later infection |
- If going home with JP drain - remove if < 100 ml/day
PAVA:
- Pre-op abx: cefoxitin
- Similar to Stanford, just 1 day slower for diet
| Diet | Pain | Other | |
| POD 0 | sips of clears IV NS@125 |
APAP, toradol, prn oxy | Neobladder: start q4h irrigation |
| POD 1 | clears | Ileal conduit: stoma visits | |
| POD 2 | fulls SLIV |
Lovenox teaching | |
| POD 3-4 |
regular | Stoma cath out POD4 |
- Ureteral stents x 1 week
Post cystectomy surveillance
- Years 1-2:
- LFTs/BMP q3-6 mo
- CT IVP q3-6 mo
- CXR/CT chest q3-6 mo
- Urine cytology q6mo
- Years 3-5: LFTs + B12, CT IVP, CXR/CT chest annually
- Years 5-10: B12, renal US to monitor for hydronephrosis annually
- PET/CT only if metastasis suspected
Video Lectures:
- Non muscle invasive bladder cancer (COViD UCSF - 1hr)
- BCG unresponsive bladder cancer (COViD UCSF - 1hr)
- Robotic radical cystectomy (COViD UCSF - 1hr)
Guidelines:
- AUA guideline – Non-muscle invasive bladder cancer
- AUA guideline – Muscle invasive bladder cancer (non-metastatic)
AUA Core Curriculum (may require login):

