Pancreatic cystic lesions
- can be isolated or a/w VHL, ADPKD
Inflammatory fluid collections - not true epithelial cysts; are local complications of acute pancreatitis. However PCNs can cause pancreatitis so do not assume cyst to be inflammatory
| Timing | Location | Definable wall | Contents | |
| Acute peripancreatic fluid collections | < 4 wks of acute pancreatitis | Extra | No | No solid/necrosis |
| Pseudocysts | > 4 wks | Extra/intra | Yes | No solid/necrosis |
| Acute necrotic collections | in setting of nec panc | Extra/intra | No | Liquid/solid |
| Walled-off pancreatic necrosis | > 4 wks | Extra/intra | Yes | Liquid/solid, with necrosis |
Non-neoplastic pancreatic cysts - rare, often asymptomatic/not requiring resection, usually diagnosed after resection of something thought to be PCN
Pancreatic cystic neoplasm (PCN)
| Pathology | Malignant degeneration | |
| Serous cystic tumors/cystadenoma 12-16%, F > 60Y |
Arise from pancreatic centro-acinar cells | Very rare, don't need to resect |
| Mucinous cystic neoplasms (MCNs) 16-23%, F > 40Y |
Mucin expressing, cellular atypia, ovarian-like stroma Tail or body, not communicating with pancreatic duct |
Yes - resect |
| Intraductal papillary mucinous neoplasms (IPMNs) 38-49%, M/F > 50Y |
Mucin expressing, cellular atypia Tail or body, causing dilation of pancreatic duct (main duct +/- branch duct) |
Main duct - yes, resect Branch duct - no, observe |
| Solid pseudopapillary neoplasms (SPNs) 3-5%, F < 35Y |
Body or tail, solid/cystic/calcifications | Yes, resect |
Diagnosis - MRI/MRCP +/- CT, EUS with FNA, CA 19-9/CEA to determine mucinous cyst
Higher risk of malignancy - size > 3 cm, main duct dilation, solid component
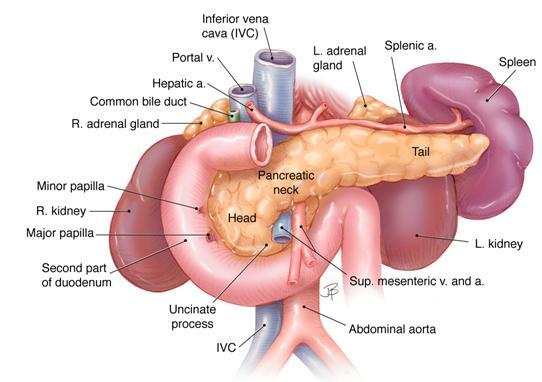
- Blood supply:
- Neck/body/tail: supplied by pancreatic branches of splenic artery; drain into splenic vein
- Head: supplied by sup/inf pancreaticoduodenal artery from gastroduodenal/SMA; drain into SMV/portal vein
- Ampulla of Vater = hepatopancreatic duct (CBD + PD) at major papilla
Whipple
- Op note
- Resection of head of pancreas requires resection of duodenum (also take 1st 15 cm of jejunum, distal stomach, gallbladder)
- Conventional - jejunum to pancreas, bile duct, and stomach
- Roux-en-Y - Jejunum to pancrease and bile cut, then 'roux'/alimentary limb between stomach and jejunum