I. Urinary Tract Infections:
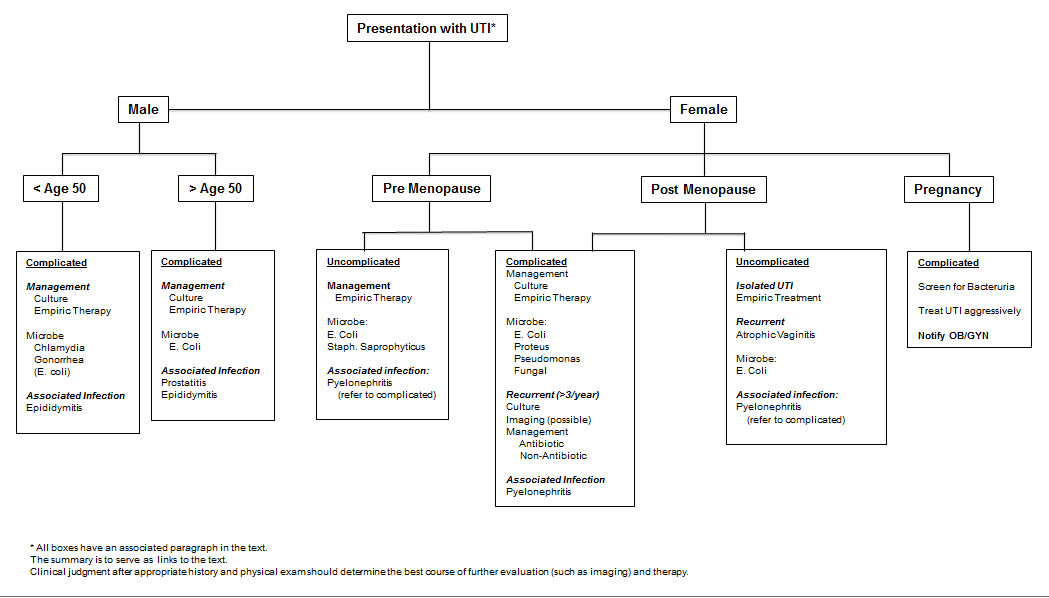
Uncomplicated UTI: Healthy female with no anatomic abnormalities.
Complicated UTI: More complicated therapy required due to:
- bacterial factors such as virulence, resistance, or unusual species
- host factors such as anatomic abnormalities, male gender, or obstruction/stasis of urine, pregnancy, immunocompromised.
Structural and functional abnormalities of the GU tract associated with complicated UTIs:
| Obstruction | Ureteric or urethral strictures |
| Tumours of the urinary tract | |
| Urolithiasis | |
| Prostatic hypertrophy | |
| Diverticulae | |
| Pelvicalyceal obstruction | |
| Renal cysts | |
| Congenital abnormalities | |
| Instrumentation | Indwelling urethral catheter |
| Intermittent catheterization | |
| Ureteric stent | |
| Nephrostomy tube | |
| Urological procedures | |
| Impaired voiding | Neurogenic bladder |
| Cystocele | |
| Vesicoureteral reflux | |
| Ileal conduit | |
| Metabolic abnormalities | Nephrocalcinosis |
| Medullary sponge kidney | |
| Renal failure | |
| Immunocompromised | Renal transplant |
Top 8 Most Common Bacterial Causes of UTI:
E coli (80%) – Staph saprophyticus – Klebsiella – Enterococcus – Group B strep – Proteus – Pseudomonas – Staph aureus
E coli P fimbria bind to urothelial cells via galactose disaccharide.
Staph aureus has hematogeneous spread, bacteriemia sources, obtain blood cultures.
Consider Non-bacterial UTIs: Candida, adenovirus, BK virus.
II. Antibiotics Table:
| Antibiotic | Mechanism | Bacterial Coverage |
|
Ampicillin, Amoxicillin
|
Disrupt cell walls | Strep, enterococcus |
|
Augmentin, Unasyn
|
Cell wall inhibitor, Beta lactamase inhibitor |
Strep, enterococcus, some GNRs, anaerobes |
|
Piperacillin/tazobactam (Zosyn)
|
Cell wall inhibitor, Beta lactamase inhibitor | Strep, enterococcus, MSSA, GNRs, anaerobes |
|
Cefazolin, Cephalexin (1st gen cephalosporin)
|
Disrupt cell walls | Gram positivies, MSSA, strep, E coli, Klebsiella, Proteus |
|
Cefoxitin (2nd gen cephalosporin)
|
Disrupt cell walls | Gram positives, GNRs, anaerobes |
|
Ceftriaxone (3rd gen cephalosporin)
|
Disrupt cell walls | Strep, GNRs, Neisseria |
|
Cefepime (4th gen cephalosporin)
|
Disrupt cell walls | GNRs, pseudomonas |
|
Ertapenem, Meropenem
|
Disrupt cell walls |
ESBL coverage (Does not cover enterococcus, pseudomonas, MRSA) |
|
Gentamicin, Amikacin, Tobramycin (Aminoglycosides)
|
Inhibit bacterial protein synthesis |
Aerobic GNRs (Gent dosing: 5-7mg/kg per 24 hours) |
|
Trimethoprim-Sufamethoxazole
|
Depletes folic acid, inhibit protein synthesis | Staph, strep, GNRs, enterobacter |
|
Ciprofloxacin, Levofloxacin (Fluoroquinolones)
|
Inhibits DNA gyrase | GNRs, pseudomonas, some gram positives |
|
Doxycycline
|
Inhibit protein synthesis | Chlamydia, mycoplasma, ureaplasma |
|
Vancomycin
|
Disrupt cell walls | Gram positives, MRSA |
|
Nitrofurantoin
|
Block carbohydrate metabolism | E coli, Staph, Enterococcus |
III. Pyelonephritis:
Bacterial infection of the renal parenchyma, often from ascending GU tract infection.
Symptoms: Flank pain, fever, CVA tenderness, dysuria
Treatment:
- Uncomplicated, no obstruction = 7-14 days of antibiotics
Ex: Cipro 500mg PO BID x 7d, Levo 750mg PO qD x 7d, Bactrim DS PO BID x 14d
2. Severe pyelo/hospitalized = IV antibiotics until afebrile, then PO antibiotics 14d
Ex: IV Ceftriaxone, Cipro, Amp/Gent
3. If associated obstruction = ureteral stent or percutaneous nephrostomy + antibiotics.
IV. Obstructive pyelonephritis:
Symptoms: fevers/chills, flank pain, nausea/vomiting, ill-appearing
CT scan: hydronephrosis, obstructing ureteral stone, perinephric stranding, urothelial enhancement
If an infected hydronephrosis is completely obstructed, the urinalysis/urine culture may be negative.
Treatment: urgent decompression with ureteral stent vs. nephrostomy tube placement.
V. Renal Abscess:
Most commonly gram negative infections, associated with renal stones, pyelonephritis, complicated UTIs.
Symptoms: Cyclic fevers/chills (not responding to antibiotics), Flank pain
CT scan with IV contrast is diagnostic test of choice.
Treatment:
- Abscess < 3cm = IV antibiotics alone
- 3-5cm = consider percutaneous drainage by IR
- >5cm = consider open surgical drainage, possible nephrectomy
VI. Xanthogranulomatous Pyelonephritis (XGP):
Chronically inflamed kidney with destruction of renal parenchyma (unclear etiology), but associated with scarring from prior infections, obstruction, immunocompromised states, and loss of renal function.
Diagnosis by histology: Lipid laden, foamy macrophages (xanthoma cells)
Treatment: Nephrectomy (usually open approach) and resection of all infected/inflamed tissue.
Optional Additional Reading:
1. Nickel, J C. (2005). Management of urinary tract infections: historical perspective and current strategies: Part 2--Modern management. The Journal of urology, 173(1), 27-32.
2. Nicolle, LE. (2005). Complicated urinary tract infection in adults. Can J Infect Dis Med Microbiol, 16(6): 349-360.