Indications
- Inadequate peripheral access
- Administer noxious meds to avoid peripheral vein irritation - pressors, chemo, TPN, etc.
- Hemodynamic monitoring - ScvO2, CVP, etc.
Types of central lines
| Central line type | Indications |
| PICC (peripherally inserted central catheter) |
Easier; more comfortable for pt (located in upper arm) AVOID in dialysis pts due to risk of thrombosing off future fistula site |
| TLC (triple lumen catheter), Hohn - non-tunneled | Common central lines with multiple lumens to draw blood/administer meds |
| Trialysis | Larger triple lumen catheter that accommodates dialysis/high flow |
| Cordis (introducer) | Large bore single lumen - "introduce" other catheters through it (e.g. Swan Ganz), or use for high volume fluid resusc |
|
Tunnelled (Hickman, Broviac) Port-a-cath |
Semi-permanent implanted central lines. Tunnelled lines are still partially external (e.g. can get tugged on). |
- Flow rate depends on catheter size and length. So PICC (small, long distance from insertion site to SVC) has slower rate than a TLC and is less preferred for high volume fluid resuscitation.
- How to insert a central line
- Typical central line length rule of thumb
- R IJ - 15 cm
- L IJ - 20 cm
- Femoral - 30 cm
- Removing a central line
- Place patient in Trendelenberg for IJ/SC (still at risk of air embolism)
- Tell patient to hum continuously (increases intrathoracic pressure to reduce venous air entry)
- Remove line quickly, inspect end of line to make sure it is intact
- Place an occlusive dressing and hold pressure for ~ 5 min
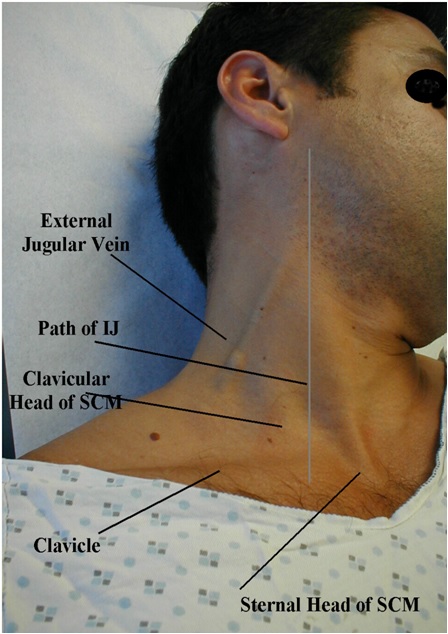
Central line locations
| Location | Pros | Cons |
|
Internal jugular
|
Most commonly used, reliable access and positioning in SVC | |
|
Subclavian
|
Lowest rate of central line infection |
Difficult to hold pressure, so coagulopathy is a relative contraindication Higher potential risk of PTX, so avoid in resp. compromise |
|
Femoral
|
Easier to access (don't need to Trendelenberg or lay flat) |
Hinders mobility With proper aseptic technique, no increased risk of infection compared to SC/IJ |


Plain films to confirm positioning
- Good interactive quiz here
| Good | Bad | |
| R IJ |
Tip at cavo-atrial junction (~ 1 cm below R main bronchus); should not enter RA or RV (can cause arrhythmia)
|
Cannulated the carotid, oops (more medial course than expected for IVC)
|
| L IJ |  |
|
| Subclavian |
Catheter passes below level of clavicle (but a/w a PTX here)
|
In subclavian artery (passes above clavicle) instead of vein; can also travel upwards into carotid artery |
| Swan Ganz |
Terminate in main pulmonary artery |
Too far in to R pulmonary artery - can cause injury |
| Femoral |
Complications
- Venous air embolism (acute hypotension, hypoxemia, cardiovascular collapse)
- Trendelenberg patients for IJ/SC lines (access point below the heart) to facilitate venous filling and reduce risk of venous air embolism
- If suspect air embolism, occlude air source, turn patient to left lateral decubitus (right side up) to prevent air from traveling from right heart to pulmonary arteries
- Call code, IVF, 100% O2, intubate, call cardiology for emergent echo to locate air embolus and aspirate
- Malpositioning
- Ideally should terminate in SVC or cavoatrial junction (higher flow; medications are less irritating to the vessel)
- ~1 cm below R main bronchus
- If line is in heart, can cause ectopy/arrhythmias
- If line is too peripheral, can cause thrombus/irritation of vessel
- Can retract a line, but can't advance after it's in (guidewire is out)
- Sometimes can flip up from SVC into the jugular (e.g. coughing causes pressure changes)
- If this is identified, shouldn't use it until fixed
- Can sometimes spontaneously resolve. Or can use power flushes (e.g. short impulses from a saline flush to create higher pressure in the jugular and cause catheter tip to flip back down).
- Arterial cannulation
- Needle stick - hold pressure. If cannot hold pressure (e.g. subclavian artery), call vascular surgery
- Dilation - occlude end of dilator (do not remove) and call vascular surgery (now have large defect in arterial wall)
- Pneumothorax
- Give 100% non-rebreather O2 and repeat chest x-ray in few hours; most small/asymptomatic ptx will spontaneously resolve
- If symptomatic/hemodynamically unstable, consider chest tube or needle decompression
- Kinking
- Venous injury - hemothorax, mediastinal hematoma
- https://psnet.ahrq.gov/webmm/case/51/crossing-the-line
- https://www.radiologymasterclass.co.uk/tutorials/chest/chest_tubes/chest_xray_central_line_anatomy
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3190489/
- https://depts.washington.edu/simcentr/cvc/extern_cvc_md/story_html5.html?lms=1


