Pathologic subtypes
- Clear cell RCC (70-80%) - most common primary renal malignancy in adults; from proximal tubule; a/w VHL
- "Clear" nature comes from glycogen/cholesterol being extracted by prep for histology
- Papillary RCC (15%) - more multifocal
- Chromophobe RCC (3-5%) - from collecting duct, a/w BHD
- Oncocytoma (benign) - similar to chromophobe/also from collecting duct; a/w tuberous sclerosis, Birt-Hogg Dube (BHD)
- Collecting duct RCC (< 1%) - aggressive, poor prognosis
- Medullary RCC (rare) - from collecting duct, a/w sickle cell patients, poor prognosis
- Mucinous tubuar and spindle cell (rare) - favorable prognosis
*Sarcomatoid variant can be a/w any subtype - poor prognosis
Risk factors: tobacco, obesity, HTN, familial (hereditary papillary RCC, VHL, BHD, tuberous sclerosis)
| Syndrome | Tumor type | Associated findings | Genetics |
| VHL | ccRCC (can arise from cystic and non-cystic tissue) |
hemangioblastoma (brain/cerebellum, spine, retina) (40-70%), pancreatic cysts/NETs, pheochromocytoma, epididymal/broad ligament cystadenoma, endolymphatic sac tumors of middle ear
|
chr 3, VHL tumor suppressor loss of function, AD |
| BHD | oncocytoma, chromophobe (or hybrid of 2) | fibrofolliculomas (cutaneous), pulmonary cysts (spontaneous hemothorax) | chr 17, BHD encodes folliculin, AD (incomplete penetrance) |
| Hereditary papillary RCC | Type 1 papillary | multiple, bilateral | chr 7, c-met oncogene, AD (incomplete penetrance) |
| Hereditary leiomyomatosis and papillary RCC | Type 2 papillary, collecting duct Aggressive - start screening age 8 (abd MRI), do not surveil |
leiomyomas of uterus and skin | chr 1, fumarate dehydrogenase (FH), AD |
| Tuberous sclerosis | angiomyolipoma | lymphangioleiomyomatosis of lung, sugar tumor of lung, pancreas and uterus, other PEComas, cardiac rhabdomyomas, subependymoas and giant cell astrocytomas and retinal hamartomas. | chr 9, TSC1/2 tumor suppressor, AD |
| Succinate dehydrogenase | Chromophobe, clear cell, type 2 papillary, oncocytoma Aggressive |
Papillary thryoid carcinoma Paraganglionomas |
succinate dehydrogenase complex subunits |
Grading: Furhman grading is used for ccRCC and papillary RCC (based on nuclear size/characteristics)
- I-IV, higher grade = worse prognosis
Staging:
| Stage I (T1N0M0) | T1* | Limited to kidney and < 7 cm in greatest dimension |
| .T1a | < 4 cm | |
| .T1b | 4-7 cm | |
| Stage II (T2N0M0) | T2 | Limited to kidney and > 7 cm in greatest dimension |
| .T2a | 7-10 cm | |
| .T2b | > 10 cm | |
| Stage III (T3N0-1M0) (Or T1-2 N1M0) |
T3 | Within Gerota's fascia and no adrenal involvement, but involving major veins or perinephric tissues |
| .T3a | renal vein, microscopic perirenal/renal sinus fat invasion | |
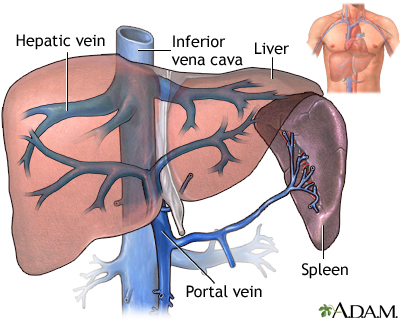
| .T3b | vena cava below diaphragm or macroscopic perirenal fat invasion | |
| .T3c | vena cava above diaphragm or invades wall of vena cava | |
| T4 any N, or any T and M1 | T4 | Beyond Gerota's fascia or involving ipsilateral adrenal gland |
| N1 | Regional lymph nodes (renal hilar, aortic, interaortocaval, caval) | |
| M1 | Distant metastasis |
*20% of T1 masses are benign (oncocytoma, AML); 60% indolent, 20% potentially aggressive
IVC thrombus (occurs in 5-10%)
- Potential surgical cure in 50-70%; not always a/w metastasis. 5 year disease-free survival ~ 65% after surgery.
- Invasion of wall (T3b) is more important prognostic factor than level. MRI can assess invasion with PPV/NPV 90%
- Mayo staging system
- Level I - adjacent to ostium of renal vein
- Level II - up to lower part of liver
- Level III - intrahepatic but below diaphragm
- Level IV - above diaphragm (requires bypass)
- MRI preferred; tumor thrombus will enhance while bland thrombus does not
- Generally put on anticoagulation
- Surgery
- Surgical tips for IVC thrombus
- Get imaging as close as possible to date of surgery (< 2 wks)
- Preop embolization - no clear benefit, unless bulky RP nodes make access to artery
- If chronic IVC collusion - avoid ligating the collaterals (lumbars through hemiazygous) that have developed. In this case don't actually need to reconstruct infrarenal IVC if taken.
- Now > 60% are found incidentally
- Classic 'triad' - hematuria, flank pain, abdominal mass - is rare now
- 15% present with locally advanced/metastatic RCC
- Can present with spontaneous perirenal hemorrhage, which may obscure underlying mass. Follow with CT a few months later - 50% of spontaneous bleeds have an occult renal tumor (AML/RCC)
Natural history
- Metastasizes hematogenously + lymphatically to lung and bone (spine). 20% of patients present with metastatic disease.
- Paraneoplastic syndromes of note:
- Hypertension (40%) - renin production, or encasement of renal artery
- Anemia (36%)
- Cachexia, weight loss, fever (15-35%)
- Stauffer's (15%) - abnormal LFTs, but not necessarily due to liver invasion/emts
- Hypercalcemia (5%) - PTHrP or lytic bone lesions
- Polycythemia (↑ erythropoietin)
- In general - 5-year cancer specific survival for T1a renal masses is > 95%. For other stages:
- T1b - 80-90%
- T2 - 50-80%
- T3b/c (IVC thrombus) - 20-50%
- Metastatic - 0-10% pre-checkpoint era, now maybe ~ 25%?
- CBC, CMP, UA
- Abdominal imaging - CT/MR pre/post contrast
- Iodinated contrast - pre-hydrate with NS if GFR < 30; consider prehydration if GFR 30-45
- Gadolinium - OK to give for GFR < 30; lower risk of NSF than previously thought
- In general - RCC enhances > 15-20 HU, does not have fat
- Chest imaging - CXR, or CT chest if thought to be high risk or has abnormal CXR
- Bone scan - only if bone pain or elevated alk phos
- Brain imaging - only if neurologic sx
- Renal mass biopsy - if suspect metastatic disease, inflammatory, infectious, or hematologic (e.g. lymphoma). Otherwise low utility.
- Genetic testing if: age < 46, bilateral multifocal disease, or family history of kidney cancer.
- Nephrology referral - if expect GFR < 30 postop; if DM with CKD. Can get Mag3 scan to predict expected GFR
Localized disease
Surveillance
- Reasonable for solid masses < 2 cm or predominantly cystic mass, or if limited life expectancy/don't want surgery
- Should treat if ≥ 3 cm, growing > 0.3 cm/year, symptoms, or biopsy shows high-grade cancer
- Repeat imaging in 3-6 mo
Ablation: for cT1a < 3 cm. Radio or cryoablation. Slightly worse outcomes wrt local recurrence.
Radical nephrectomy (RN): removal of Gerota's fascia (containing kidney and perirenal fat)
- Remove adrenal if: upper pole tumor > 7 cm, tumor thrombus involving, imaging/intraoperative suspicion of adrenal involvement. Adrenal insufficiency rare if contralateral adrenal is OK
- Regional lymph node dissection: only if there is clinically concerning lymphadenopathy. Does not improve cure/survival for T1-T3N0M0; maybe for N1.
- L - para-aortic + interaortocaval; R - paracaval + interaortocaval. Template: from diaphragm crus to common iliac.
- Adjuvant therapy for high risk of recurrence: Many negative studies pre-IO, but FDA approved for
- Stage II (T2N0) Gr 4 clear cell +/- sarcomatoid - pembrolizumab
- Stage III (T3 or N1) clear cell - pembro (or sunitinib - less evidence)
- KEYNOTE-564 (pembro, 2021) positive study (disease-free survival 77% vs 68% at 24 mo), but atezo and nivo were negative studies
- ASSURE nomogram for cancer-free survival
Nephron sparing (NSS): Partial nx, enucleation, or ablation; less hit to GFR. Use if renal mass ≤ 7 cm (eg T1, similar cure rate as RN), or need to preserve more kidney function (solitary, poor renal function, b/l tumors).
- Local recurrence after PNx for small renal masses in < 2%
- Consider ablation (thermal, radio, cryo) for solid masses < 3 cm.
- Should do biopsy prior to (preferred) or during ablation for pathologic confirmation.
- Should get pre/post contrast imaging within 6 mo after ablation (5-10% failure rate for ablation)
If GFR < 45 or expected to be < 30 after intervention, consider referral to nephrology
- EORTC 30904 - PNx reduces incidence of moderate renal dysfunction (GFR < 60), but PNx/RNx equivalent incidence of severe dysfunction (GFR < 30, GFR < 15)
- PNx on solitary kidney - 5-15% required temporary dialysis, 5% required permanent dialysis
- If microscopic margins positive, increase risk by one level
- Follow-up intervals (in months) below based on risk
- H&P
- Abdominal imaging (CT or MR abdomen, pre+post contrast). Can switch to US after 5 years or after 2 years in LR/IR groups
- Chest imaging (CXR (LR/IR) or CT chest (HR/VHR)). Can switch to CXR after 5 years for HR/VHR groups.
- 30% of recurrences are diagnosed after 5 years. After 5 years, informed/shared decision-making should dictate further abdominal imaging.
- After ablation - abdominal CT or MRI with and without IV contrast at 6 mo following ablation, then according to intermediate risk protocol
| Recurrence rate | 3 | 6 | 9 | 12 | 18 | 24 | 30 | 36 | 48 | 60 | 72-84 | 96-120 | |
| Low risk (LR) pT1 Gr 1/2 |
6-15% | x | x | x | x | x | x | ||||||
|
Intermediate risk (IR) |
20-30% |
x | x | x | x | x | x | x | x | ||||
|
High risk (HR) |
50% |
x | x | x | x | x | x | x | x | x | x | ||
|
Very high risk (VHR) |
65%-75% |
x | x | x | x | x | x | x | x | x | x | x | x |
Advanced disease
Systemic therapy
- Mainstay is immunotherapy + checkpoint inhibitors - chemo generally ineffective
- Risk stratification for advanced disease: IMDC (International Metastatic RCC Database Consortium)
- Risk factors: Karnofsky performance status < 80%, time from diagnosis to treatment < 1 year, Hgb < LLN (12), calcium > ULN, ANC > ULN, platelets > ULN, LDH > 1.5x ULN (MSKCC)
- 0 risk factors - favorable risk (44mo survival)
- Limited disease burden
- Can consider close active surveillance
- Single-agent anti-angiogenic (sunitinib or pazopanib)
- Single-agent immunotherapy (pembro or nivo)
- Substantial disease burden - immuno + anti-angiogenic, or combo immuno
- Nivolumab + ipilimumab
- Pembro + axitinib
- Nivolumab + cabozantinib
- Limited disease burden
- 1-2 risk factors - intermediate risk (27mo survival), ≥ 3 risk factors - poor risk (9mo survival)
- Symptomatic or life threatening disease - lenvatinib + pembro, or nivolumab + cabozantinib
- Otherwise - above options plus nivolumab + ipilimumab, pembro + axitinib
- 1st line poor performance: temsirolimus
Classes of therapies
- PD-1 checkpoint inhibitors (pembrolizumab, nivolumab (2015))
- PD-L1 checkpoint inhibitors (avelumab, atezolizumab)
- Anti CTLA-4 antibody (ipilimumab)
- mTOR inhibitor (tumor cell growth/survival inhibitors) (everolimus (2008), temsirolimus (2007) for non-ccRCC)
- Decreases VEGF (angiogenesis), HIF (cell proliferation)
- VEGF tyrosine kinase inhibitors (TKI) (axitinib, sunitinib, pazopanib, cabozantinib, lenvatinib, bevacizumab)
- Toxicity: HTN, impaired wound healing, GI perforation, hand/foot/mouth mucositis
- Soarafenib, sunitinib (2005-2006)
- Pazopanib - same response as sunitinib; less side effects
- Cabozantinib - superior survival to sunitinib (46% response vs 18%)
- Bevacizumab - stop bevacizumab 28 days before/after surgery for wound healing.
- Nivolumab + ipilimumab
- FDA approved (2020) for first line for intermediate/poor risk, used off label for favorable risk
- Checkmate 214 trial: nivo/ipi vs sunitinib. Intermediate/poor risk - complete response 9% vs 1% (~40% of these had durable response). 5-year OS 43% vs 31%, 5-year PFS 31% vs 11%. (for favorable risk - similar OS, lower PFS, higher CR).
- Pembro + axitinib
- FDA approved (2019) for first line treatment regardless of risk
- KEYNOTE-426 trial: pembro/axi vs sunitinib. Entire cohort: complete response 9% vs 3%. 2-year OS 74% vs 65%, 2-year PFS 38% vs 27%.
- Nivolumab + cabozantinib
- FDA approved (2021) for first line treatment regardless of risk
- CheckMate 9ER trial: nivo/cabo vs sunitinib. Entire cohort: complete response 12% vs 5%. 2-year OS 70% vs 60%, 2-year PFS 40% vs 21%.
- Lenvatinib + pembrolizumab
- FDA approved (2021) for first line treatment regardless of risk
- CLEAR trial: nivo/cabo vs sunitinib. Entire cohort: complete response 16% vs 4%. Improved OS, PFS 24mo vs 9mo
- Avelumab + axitinib vs sunitinib - improved PFS but not OS
- Second line therapy - depends on how long first agent worked and what they had before
- If failed TKI - can try another TKI or IO. Cabozantinib superior to everolimus (METEOR trial)
- If failed IO - use a TKI
- General principles
- Tumor may look larger initially due to infiltration of T cells - wait 3 mo for first scan; may take 6 mo to start shrinking
- Can have flares of autoimmune conditions (eg mostly anything besides autoimmune thyroiditis)
- Older agents
- High dose IL-2 (durable remission for ccRCC in only 3-5%) - stimulates cell-mediated immunity. Very toxic (vascular leak, syndrome, renal failure, arrhythmias)/high mortality (1990s). Need to have high performance status; not used much anymore
- Interferon alpha - no longer manufactured
Metastatectomy
- Solitary metastasis or oligometastasis: resect if can render disease free with resection.
- Lung metastasis has better prognosis than other locations.
- 44% 5-year survival for complete metastectomy vs 10-15% if not
- Bone met > 3cm in weight-bearing bone - ortho surgery before systemic therapy
Cytoreductive nephrectomy
- Intermediate/poor-risk patients: should do upfront systemic therapy.
- If complete reponse, -> cytoreductive nephrectomy
- If stable or partial response, can consider cytoreductive nephrectomy
- Progression -> no nephrectomy
- Poor risk or worsened performance status -> no nephrectomy
- Data
- Interferon era - data supported cytoreductive nephrectomy prior to IFN/IL-2, but these are no longer used
- TKI/Anti-angiogenic era
- CARMENA trial showed upfront nephrectomy + sunitinib not superior to sunitinib alone (however trial included many poor risk patients)
- IO/Checkpoint inhibitor era - no prospective data yet, but SWOG 1931/PROBE trial underway to study IO followed by cytoreductive nephrectomy (if stable or partial reponse to IO) vs IO alone
- Delayed nephrectomy benefits - SURTIME trial - deferred nx improved OS by 17.4 mo compared to immediate nx.
- Antigen load may help IO work better, and can identify those who wouldn't benefit from nephrectomy (disease progression on IO)
- Upfront cytoreductive nephrectomy more likely to benefit: good performance status, lung-only metastases
Pocket urology - page 21